Bernal-Mizrachi Lab
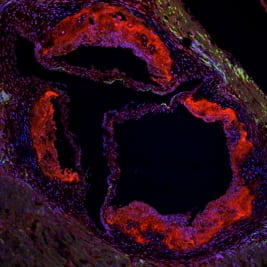
The long-term goal of our laboratory is to determine the mechanisms responsible for metabolic syndrome and its vascular complications. We are particularly interested in understanding the mechanisms of the interactions between vitamin D signal transduction, intracellular calcium, and endoplasmic reticulum stress in critical tissues responsible for the development of metabolic syndrome and its complications.
Characterization of the effects of vitamin D deficiency on the development of metabolic syndrome and vascular complications
The long-term goal of our laboratory is to determine the mechanisms responsible for metabolic syndrome and its vascular complications. We are particularly interested in understanding the mechanisms of the interactions between vitamin D signal transduction, intracellular calcium, and endoplasmic reticulum stress in critical tissues responsible for the development of metabolic syndrome and its complications. We and others have shown that vitamin D treatment improves factors linked to vascular inflammation in patients with metabolic syndrome: it improves peripheral insulin action, suppresses the renin angiotensin system, decreases systemic inflammatory mediators, decreases macrophage cytokine release, and prevents macrophage cholesterol deposition by downregulation of endoplasmic reticulum stress. In our laboratory, we have generated mouse models of diet-induced vitamin D deficiency and engineered mice with altered vitamin D receptor and endoplasmic reticulum stress signaling in order to identify the role of this vitamin in different tissues involved in the development of metabolic syndrome and vascular inflammation.
Identification of signaling pathways controlling macrophage phenotype and function
Macrophages play a critical role in the development of metabolic syndrome and atherosclerosis. Monocytes recruited to the subendothelial space at sites of endothelial cell activation respond to environmental signals and differentiate into macrophages with diverse functional programs. We are identifying the effects of different environmental conditions on signaling pathways that regulate monocyte/macrophage differentiation and function in patients with type 2 diabetes. We also use genetically-modified mouse models to dissect the signaling pathways implicated in cellular differentiation, cholesterol deposition, and inflammatory responses.
Translation of Basic Science Results into Human Trials
We are actively enrolling patients into two clinical trials of patients with type 2 diabetes to assess the effects of vitamin D supplementation on blood pressure and subclinical markers of cardiovascular disease. For more details or if you are interested in participating, please see “Clinical Studies” page.
Current Clinical Studies
Vitamin D and Blood Pressure (VDBP)
What is the VDBP clinical study?
The objective of this study is to evaluate the effects of vitamin D on blood pressure control and vascular disease in vitamin D-deficient patients with type 2 diabetes and hypertension.
Why are we doing this study?
In recent years, vitamin D has been shown not only to be important for bone and calcium metabolism but also in other tissues involved in vascular disease in patients with diabetes. Epidemiological studies demonstrate high rates of vitamin D deficiency in patients with type 2 diabetes and suggest an increased risk of cardiovascular disease and hypertension with low vitamin D levels.
Who should call to inquire about the study?
You may be eligible for the study if you are 25-80 years old with type 2 diabetes not requiring insulin and mildly elevated blood pressure. You can be on any blood pressure medications.
Who will be eligible to participate in VDBP study?
After the results of the screening visit are back, we will let you know if you qualify for the study. To be eligible for the study you must have a low vitamin D level, mildly elevated blood pressure, and reasonably-managed diabetes.
What will I be asked to do as a participant?
The VDBP clinical study will determine whether supplementing vitamin D in patients with type 2 diabetes that have low vitamin D levels decreases blood pressure over a 4 month period. Over that period, you will be randomized to take either 4,000 units of vitamin D3 or placebo daily, in addition to calcium supplements. At the study visits, we will do blood and urine tests, blood pressure monitoring, and ultrasounds of your blood vessels. There are 8-9 study visits, including the screenings for the VDBP clinical study.
Please contact us for more information.
Study Investigators: Carlos Bernal-Mizrachi, MD and Amy Riek, MD
Study Coordinator: Robin Bruchas, MSW
VitaminDstudy@dom.wustl.edu or (314)362-0934
Vitamin D, Cardiovascular Disease, and African Americans (VDCVD)
What is the VDCVD clinical study?
The objective of this study is to evaluate the effects of vitamin D on markers of subclinical cardiovascular disease in vitamin D-deficient African Americans with type 2 diabetes.
Why are we doing this study?
African-Americans have higher rates of both cardiovascular disease and low vitamin D levels. Multiple observational studies have showed an increased risk of vitamin D deficiency in African Americans with type 2 diabetes, in addition to correlation between cardiovascular disease and vitamin D levels. However, no clinical studies have tested whether treating with vitamin D will reduce cardiovascular disease in this population.
Who should call to inquire about the study?
You may be eligible for the study if you are 50-80 years old and African-American with type 2 diabetes.
Who will be eligible to participate in VDCVD study?
After the results of the screening visit are back, we will let you know if you qualify for the study. To be eligible for the study you must have a low vitamin D level, stable diabetic therapy (oral medications, insulin, or a combination), and reasonably controlled blood pressure and cholesterol.
What will I be asked to do as a participant?
The VDCVD clinical study will determine whether supplementing vitamin D in African Americans with type 2 diabetes that have low vitamin D levels improves markers of cardiovascular disease over 1 year. You will be randomized to take either 4,000 units or 600 units of vitamin D3 daily in a multivitamin, in addition to calcium supplements. At the study visits, we will do blood and urine tests to look for markers of systemic inflammation, as well as ultrasounds of blood vessels, specifically to look at the thickness of blood vessels in the neck. There are 9-10 study visits, including the screenings for the VDCVD clinical study.
Please contact us for more information.
Study Investigators: Carlos Bernal-Mizrachi, MD and Amy Riek, MD
Study Coordinator: Robin Bruchas, MSW
VitaminDstudy@dom.wustl.edu or (314)362-0934
Other Links for More Information:
Volunteer for Health
https://vfh.wustl.edu/currentstudies/studies.aspx?keywordsearch=Bernal
* This links to a page within the Washington University Volunteer for Health site that is specific to the studies described above. The link below is provided for your convenience should you wish to fully navigate the Volunteer for Health site from its main page.
* To manually locate Dr. Bernal-Mizrachi’s studies within the Volunteer for Health site, click “Browse Current Studies” located towards the bottom right corner of the page. In the “My Search Criteria” window, enter “Bernal” (no quotations) and click the “Find” button.
http://www.clinicaltrials.gov/
*The above is a link to the national registry for clinical trials, ClinicalTrials.gov, which lists the two ongoing clinical studies
Principal Investigator

Carlos Bernal-Mizrachi, MD
Chief of Medicine at the Veterans Affairs St. Louis Health Care System and Professor of Medicine
- Phone: 314-362-0947
- Fax: 314-362-7641
- Email: cbernal@nospam.wustl.edu

Kevin Bauerle, MD, PhD
Instructor in Medicine
- Phone: Veteran Affairs 314-652-4100 x57640
- Email: bauerlek@wustl.edu





Amy Riek, MD (she/her/hers)
Associate Professor of Medicine and Medical Director of Clinical Operations
- Phone: 314-362-3500
- Fax: 314-747-3963
- Email: aeriek@wustl.edu

Rong Mei Zhang, MD
Instructor in Medicine
- Phone: 314-362-3500
- Fax: 314- 747-3963
- Email: rongmeizhang@wustl.edu
Oh J, Riek AE. Darwech I, Funai K, Shao, JS, Chin K, Sierra OL, Ostlund RE, Bernal-Mizrachi, C. Deletion of Macrophage Vitamin D Receptor Promotes Insulin Resistance and Monocyte Cholesterol Transport to Accelerate Atherosclerosis in Mice. Cell Reports. 2015;(15):2211-1247.
Riek AE, Oh J, Darwech I, Moynihan CE, Bruchas RR, Bernal-Mizrachi C. 25(OH) vitamin D suppresses macrophage adhesion and migration by downregulation of ER stress and scavenger receptor A1 in type 2 diabetes. J Steroid Biochem Mol Biol. 2014;144:172-179. PMID:24184871
Riek AE, Oh J, Bernal-Mizrachi C. 1,25(OH)2 vitamin D suppresses macrophage migration and reverses atherogenic cholesterol metabolism in type 2 diabetic patients. J Steroid Biochem Mol Biol. Published online ahead of print Jan 17, 2013.
Weng S, Sprague JE, Oh J, Riek AE, Chin K, Garcia M, Bernal-Mizrachi C. Vitamin D deficiency induces high blood pressure and accelerates atherosclerosis in mice. PLoS One. 2013;8(1):e54625.
Riek AE, Arbelaez AM, Bernal-Mizrachi C. Vitamin D deficiency. In Baranski TJ, Clutter WE, McGill JB, editors. The Washington Manual Endocrinology Subspecialty Consult. 3rd edition. Phildelphia, PA: Lippincott Williams & Wilkins; 2013:195-212.
Riek AE, Oh J, Sprague JE, Timpson A, de Las Fuentes L, Bernal-Mizrachi L, Schechtman KB, Bernal-Mizrachi C. Vitamin D suppression of ER stress promotes and anti-atherogenic monocyte/macrophage phenotype in type 2 diabetic patients. J Biol Chem. 2012;287(46):38482-94.
Oh J, Riek AE, Weng S, Petty M, Kim D, Colonna M, Cella M, Bernal-Mizrachi C. Endoplasmic reticulum stress controls M2 macrophage differentiation and foam cell formation. J Biol Chem. 2012;287(15):11629-41.
Riek AE, Oh J, Bernal-Mizrachi C, Vitamin D regulates macrophage cholesterol metabolism in diabetes. J Steroid Biochem Mol Biol. 2010;121(1-2):430-3.
Mulligan ML, Felton SK, Riek AE, Bernal-Mizrachi C, Implications of vitamin D deficiency in pregnancy and lactation. Am J Obstet Gynecol. 2010;202(5):429.e1-9.
Oh J, Weng S, Felton SK, Bhandare S, Riek A, Butler B, Proctor BM, Petty M, Chen Z, Bernal-Mizrachi L, Bernal-Mizrachi C, 1,25(OH)2 Vitamin D inhibits foam cell formation and suppresses macrophage cholesterol uptake in patients with type 2 diabetes. Circulation. 2009;120(8):687-698.
Bernal-Mizrachi C, Xiaozhong L, Yin L, Knutsen RH, Howard MJ, Arends JJ, DeSantis P, Coleman T, Semenkovich CF. An afferent vagal nerve pathway links hepatic PPAR alpha activation to glucocorticoid-induced insulin resistance and hypertension. Cell Metabolism, 5(2):91-102, 2007. PMC1899170
Bernal-Mizrachi C, Gates AC, Weng S, Imamura T, Knutsen RH, DeSantis P, Coleman T, Townsend RR, Muglia LJ, Semenkovich CF. Vascular respiratory uncoupling increases blood pressure and atherosclerosis. Nature, 435(7041):502-506, 2005.
Bernal-Mizrachi C, Weng S, Feng C, Finck BN, Knutsen RH, Leone TC, Coleman T, Mecham RP, Kelly DP, Semenkovich CF. Dexamethasone induction of hypertension and diabetes is PPAR-alpha dependent in LDL receptor-null mice. Nature Medicine, 9(8):1069-1075, 2003.
For a quick link to my current publications in PubMed, please click here:
PubMed
Lab Photos







